Hercule’s Pancreatitis Story
Hercule’s Pancreatitis Story
This page will share, in detail, what we went through with Hercule’s pancreatitis over the years.
The story does not have a traditionally happy ending – Hercules did end up crossing the rainbow bridge – but in sharing his story and what we have learned, we hope to provide others with resources that they can bring to their vets to help with discussions and action plans if they find themselves faced with similar circumstances.
Pancreatitis is not always deadly; but in some instances it can be. Early intervention is key – let’s share how we did that so you can learn too.
What is feline pancreatitis?
Feline pancreatitis is inflammation of the pancreas in a cat. Pancreatitis can happen to other species, including dogs and humans, but there are nuances within how each species experiences pancreatitis as well as why it has occurred. This means that just because pancreatitis may be caused by a high fat diet and alcohol use in humans, doesn’t mean that’s the case for cats.
There is no known etiology for why pancreatitis happens in cats; however, there does not appear to be a link between high fat diets and pancreatitis like there are in other species. More research is still required to find the true risk factors, but we’ll touch on that later on.
Feline Pancreatitis Attack #1 – February 2016
In 2016, Hercules found himself at the vet with a history of vomiting, diarrhea, lethargy and behaviour changes. It first started with some diarrhea but it hadn’t affected his appetite. Then his appetite was affected and he wouldn’t finish his food. After that, he didn’t want his food at all and what he did eat, he would vomit.
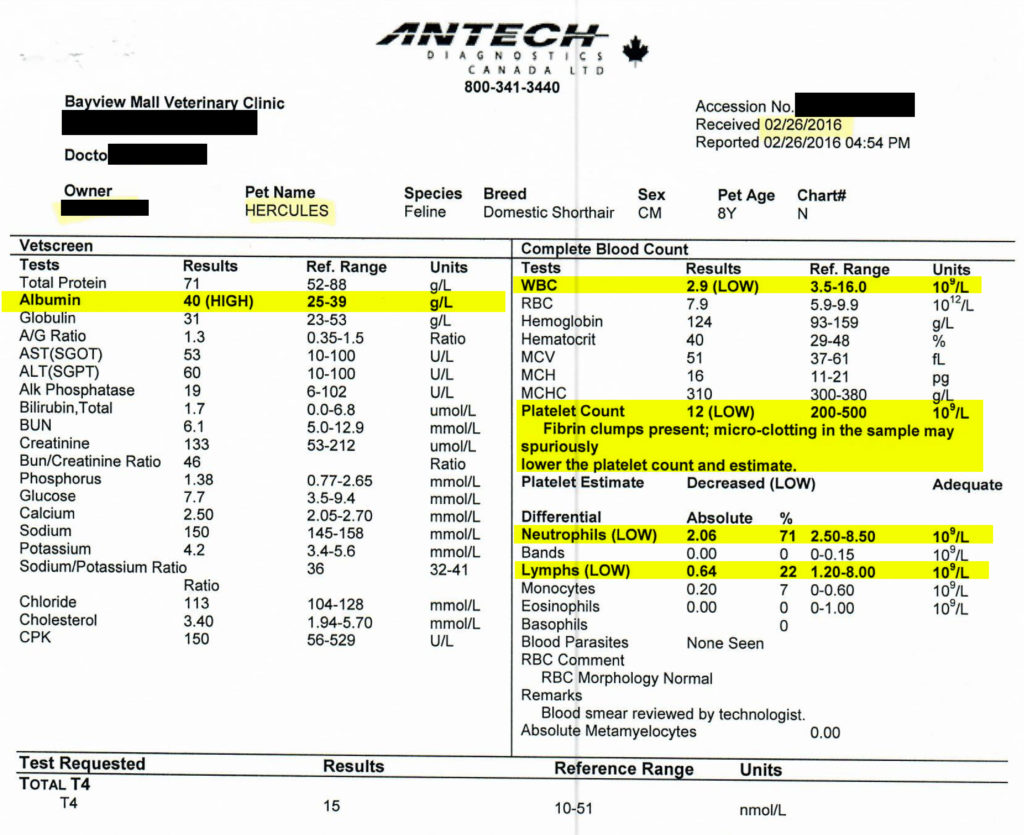
When we went to the vets, they did some bloodwork and took an x-ray to check for any blockages or obvious signs of problems. The bloodwork showed:
- Increased Albumin
- Low WBC (white blood cell)
- Low Platelets with clumping (not uncommon in cats, though)
- Low Neutrophils
- Low Lymphocytes
The x-ray showed a significant amount of gas in his GI tract but other than that, was unremarkable. Hence why we refer to that day as the $500 fart.
At the time, his symptoms were attributed to an upset tummy due to new food and gave us several cans of the Royal Canin Recovery cat food to help him eat without further adding to his indigestion. We also discussed putting Hercules on a diet and how once he was done with the Recovery food, we would switch him to the Purine O/M and provide him with a strict amount of carefully calculating calories per day.
Only when looking back on his history now as well as his bloodwork and clinical symptoms, this was actually his first pancreatitis attack.
We were told that if anything changes that we can bring him back and they can do an ultrasound, but that it should recover in a few days.
After a handful of days, he went back to normal and his appetite returned. The Recover food did the trick!
Feline Pancreatitis Attack #2 – February 2019
Just shy of 3 years to the day, Hercules prevented to the vet with the same symptoms as he did in 2016; vomiting, diarrhea, lethargy and behaviour changes. We saw a different vet this time (Cheryl – the one who was helping to manage Herc’s weightloss) and she suspected pancreatitis. She said that we can do some bloodwork to double check but that treatment for acute feline pancreatitis is mainly supportive.
The goals of managing feline pancreatitis are to address:
- Dehydration
- Nausea
- Pain
- Nutrition
Dehydration is important to manage because fluid loss can affect blood pressure. Often times fluids are given under the skin (subcutaneously) to help increase fluid levels. The dehydration is primarily due to the vomiting and diarrhea; these also need to be managed as to prevent further dehydration. A medication called Cerenia is often used and is what Hercules got. Cerenia is also known to help with pain although in more severe cases, some cats will get additional pain medication. Metronidazole can be used in addition to Fortiflora to help manage diarrhea which can also be a result of the nausea. Finally, nutritional support is key to successful management.
The sooner a cat gets back to eating normally, the sooner the pancreas can begin healing. We were given the Hill I/D canned cat food for Hercules because it’s easily digestible. The more easy it is to digest the food, the less enzymes the pancreas needs to product to aid with digestion. This will allow for the pancreas to heal itself. Sometimes cats will still have difficulty eating and an appetite stimulate is required or even a feeding tube; luckily Herc enjoyed the I/D food and began eating on his own.
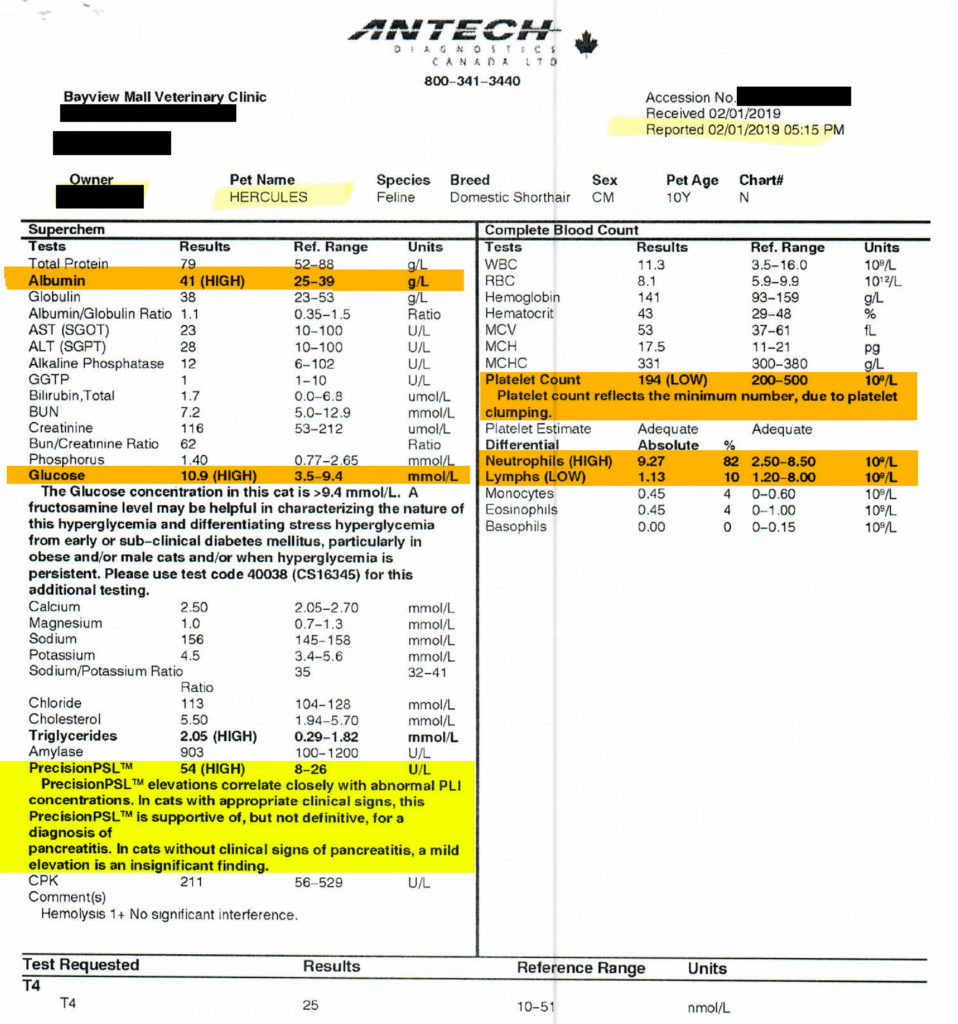
While Herc was at home recovering with supportive care, his bloodwork came back. His blood results showed:
- Increased Albumin
- Platelet count low (but no clumping noted this time)
- High neutrophils
- Low lymphocytes
- High glucode (although his fructosamine was normal)
- …and a PrecisionPSL value twice that of the normal value
The PrecisionPSL value was the key to the diagnosis. That value of the pancreas specific lipase – an enzyme that is secreted by the pancreas. High values, in combination with the signs a cat presents with, are indicative that pancreatitis is likely the underlying issue.
Given that we had our answer and Herc had now recovered from the acute attack, we asked the vet about what would happen next. She said that if he can stave off another attack for about 3-months, then we can breath a little easier. If he has another attack within 3 months then we’ll need to do more diagnostics to learn more about what’s happening and why it’s happening.
We kept him on the I/D food, knowing that cats are very good at hiding their symptoms from us, even though he ‘seemed normal’ because we wanted to make sure that everything was healing well with his pancreas. Slowly we started working some O/M back in, a tablespoon at a time as to not upset his tummy.
We were watching the days go by, anxiously awaiting for that coveted 90-day mark when we would be ‘all clear’.
Feline Pancreatitis Attack #3: April 2019
Only 50 days later, we found ourselves dealing with another bout of vomiting, diarrhea and lethargy. This time we were able to give him the Cerenia right away (since we had started keeping an emergency supply on hand) as well as Fortiflora for diarrhea and metronidazole. We called the vet and booked an appointment to have him looked at and to get more meds. A repeat of 2-months prior.
With meds in hand, we also scheduled an abdominal ultrasound for Hercules. This was quite the production since he had to be sedated. Like, really sedated. The kind of sedation where you’re given a reversal to help you wake up. Hercules detested his vet and especially his vet tech Rebecca. Even when Hercules was feeling ill and suffering from pancreatitis, he always found his spice and made sure Rebecca knew who was boss in their relationship. The ultrasound was performed
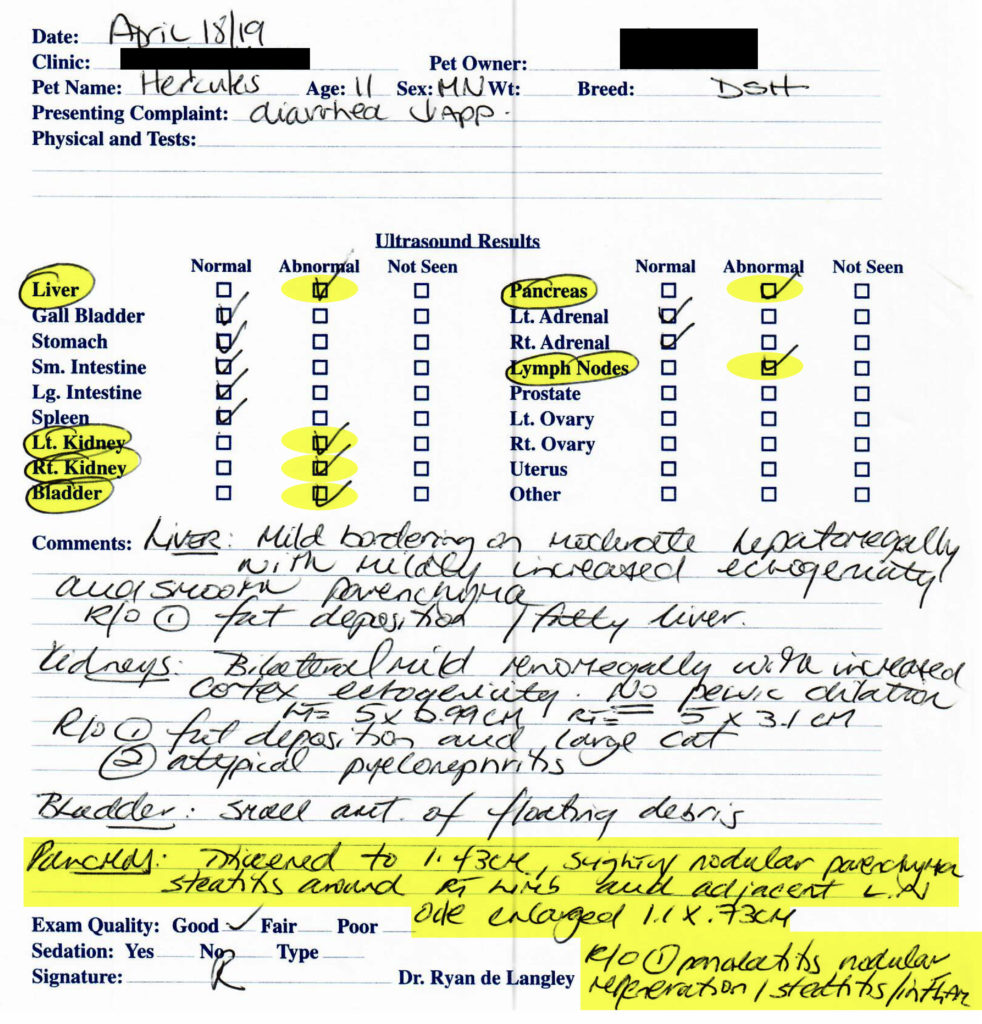
The report confirmed indications of pancreatitis and ruled out other things like IBD, cancer or other GI problems like urinary tract blockages or infections that could be setting off the pancreatitis. There were some fatty deposits in his liver which was to be expected given his size, but we were seeing success on his diet and persevering in that sense and had a plan. The ultrasound did show steatitis around the right limb of the pancreas and adjacent lymph node as well as a slight nodular appearance to the pancreas.
Steatitis us an inflammation of fatty tissue and while it can be a disease in and of itself, it’s also secondary to other things like pancreatitis.
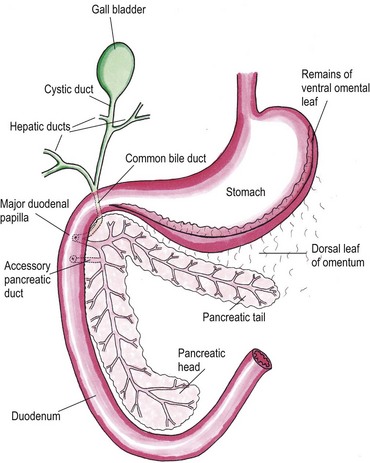
In cats, the pancreas is an L-shaped organ and the right side of it hugs the duodenum. There is always 1 duct that drains from the pancreas into the duodenum (the major duodenal papilla) and in only a small percentage of cats, a secondary accessory pancreatic duct exists. Most cats only have the 1 duct and this duct drains both the gallbladder and the pancreatic enzymes into the intestines.
In terms of nodules in the pancreas, this is something that can be observed in pancreatitis. The nodules are not tumours, rather, they are pseudocysts that are areas where the pancreatic enzymes have been encapsulated/trapped by the body so that they don’t leak out into the rest of the body and cause more damage. In a sense, they’re a representation of how your body tried to fight pancreatitis. Typically they resolve on their own once the acute pancreatitis attack has passed.
Once we understood what was going on and that Herc did not have any other underlying issues that we need to deal with (like cancer or IBD) we got some more of the I/D food and started the healing process again, anxious awaiting the coveted 90-days where we could breath easier.
Managing Chronic Pancreatitis – 2019 + 2020
While Herc hadn’t had a full on flare-up of acute pancreatitis since April of 2016, there were many instances where we would notice softer stools or vomiting without a hairball. In those cases we would either use Fortiflora for a few days and monitor, or give Hercules a Cerenia and monitor. We always had a supply on hand in the event that Herc would have a flare-up.
During the few instances where we would be away for more than 24 hours and need someone to come by and feed the cats, we had a list of all the “What to look for” signs in Hercules, instructions on meds, vet numbers and emergency contacts in the event Herc got sick. Thankfully he didn’t have any acute flareups after his ultrasound.
Feline Pancreatitis Attack #4 – December 2021
Hercules turned 13 in 2021 and he was my ‘old boy’. As his birthday rolled around, I would find myself saddened by the thought of wondering what Herc’s final years would be like. Would he end up diabetic due to his weight? Would he be immobile from arthritis? Would he just loaf somewhere all day and we would need to carry him everywhere as proper peasants would – uh, I mean pet owners? Herc was my baby and the thought of being without him was simply too much to bear. In all my anxieties; however, I never thought that pancreatitis is what would be Herc’s final chapter.
Up until this point, I did a reasonable amount of research about feline pancreatitis but noticed that there was very little out there on the internet. I found some basic resources to understand the disease in it’s acute phase but I never took the time to understand how pancreatitis can set the stage to take a life.
The story is more detailed here; but the summary is this:
Hercules vomited on Monday afternoon, we anticipated another flare of up acute pancreatitis and gave him antinausea meds and I/D food. We made a vet appointment for the next day for a checkup. He ate breakfast the next day without vomiting so that was a great sign! The checkup was unremarkable and we were given more meds and told that we caught it early and to keep doing what we were doing. That night, things changed quickly.
Hercules regressed and no longer wanted to eat – not even Temptations or Churu. He threw up after the administration of medication and a significant amount of liquid (for size reference, the puddle on the floor was larger than a dinner plate) that was not only yellow in colour but incredibly foul smelling. As the sun was about to rise and the vet clinic about to open, I noticed some open mouth breathing and while I know that’s not a good sign I also recall having seen it in the week or so prior for very short amounts of time. I had actually wondered is Herc was becoming asthmatic as I would see him do that after moving. It was only a few breaths and went away – same as that night. We ended up at the vet office as the first patient to arrive. Being COVID times, I then drove home and anxiously awaited a call from the vet with news.
I don’t recall how many times the vet phones – it was 2 or 3 and with each phone call things were looking more dire. One of the first call came in with a description of Herc’s vitals. He was breathing rapidly (tachypnea) and now had a fever. The doctor recommended and an x-ray and bloodwork and if that wasn’t conclusive then to consider an ultrasound. (Thankfully the ultrasound tech was going to be in that day – a true stroke of luck). We gave the ok for all of that.
The bloodwork wasn’t promising – lymphocytes, eosinophils and PCT were low. His creatinine was high and his lipase was through the roof. The bloodwork, with combined with the presentation of a fever, could indicate an infection or severe immune response and the high lipase and creatinine were indicative of pancreatitis and the creatinine could indicate some kidney issues, shock or dehydration.
The focus: Find out why he’s having an immune response or where the source of an infection may be.
Was an infection triggering the pancreatitis? If so – we wouldn’t be able to address the pancreatitis unless we fixed the infection. Was the pancreatitis causing an infection? We needed to learn more.
The x-ray results came in. The x-rays hosed aerophagia, which is air in the stomach, as well as a significant amount of liquid in his stomach. There was also some increased desnsities with busy looking interstitial patterns in his lungs near his heart and in the middle lobe of the right lung. Despite these densities, no edema or effusion was present (water between the layers of the lungs or around/on/in the lungs).
We needed to keep looking so the ultrasound was performed. His pancreas was difficult to visualize and delineate. There wasn’t a “clear edge” to the pancreas the way there would normally be. This can indicate that the organ is breaking down. The pancreas also showed several substantial nodules. There were other areas of inflammation within his abdomen but his pancreas was in rough shape – the ultrasound was indicative of exceptionally advanced pancreatitis.
The decision we faced
Once all the information was presented, this is what we knew:
- Hercules had pancreatitis
- There was an infection present – likely sepsis
- There was air and fluid accumulating in his stomach
- There were areas of concern in his lungs
- He was dehydrated and nauseous
- He likely was in absolutely tremendous pain
While we knew that these issues were present, we didn’t know the why. Why did he have gas and liquid in his stomach? Was that somehow caused by pancreatitis? What about the issue with his lungs? There’s no way that could have been pancreatitis, could it? That sounded outrageous.
We were left with a few possibilities to consider:
- Everything was due to the pancreatitis – if we could fix the pancreatitis then we may be able to fix the damage the attack had done to the other organs
- There’s no guarantee it’s even from pancreatitis
- There’s no guarantee or even any indication of how “fixable” the situation is
- Even if he made it through in the short term, the likelihood of severe damage to his pancreas would be substantial (which would be diabetes + pancreatic enzyme insufficiency – so more meds for the rest of his life)
- There’s no guarantee that another flare it wouldn’t happen in a few days or weeks
- Everything was due to something else, other than pancreatitis – but that the pancreatitis flared up because of this other problem – possibly cancer
- If Herc had IBD which became lymphoma or if he had a form of quick and aggressive adenocarcinoma, it’s possible that the inflammation from that induced pancreatitis
- It’s also possible that the issues with his stomach and lungs were a result of metastasis
- There was no guarantee that this was cancer, though – just a working theory
- Even if we tried to treat the pancreatitis and made it through this, we would then have to treat the cancer
- Cancer that is that far advanced upon clinic presentation would not have a positive outcome or one that would provide us any significant amount of time together
Given those two horrible scenarios, we discussed what “treating it” would look like – and regardless of the underlying issue being pancreatitis, cancer or another issue that wasn’t discussed, Hercules would need an esophigastric feeding tube (a tube that goes into the side of his neck and into the stomach) as a means of draining the fluid that is accumulating and feeding him. Without getting calories in, Hercules was facing hepatic lipidosis which is almost always fatal. After the feeding tube, Hercules would require significant IV fluids, anti-inflammatory medication and pain medication. He would need to be monitored ideally in an ICU setting or be transferred back and forth from the emerge clinic to the main vet each night as the emerge clinic provides overnight care.
This would have been a minimum of $10,000 just for care in the days ahead – this wouldn’t include the follow up care necessary including additional ultrasounds in the coming weeks. I didn’t have that kind of money, but if there was any reasonable chance of survival and a good quality of life post-survival, I would have found a way to get the money. The reality of the situation was, however, that the prognosis was grim.
I didn’t want to say the words. If I said the words out loud then it would make it so much more real.
But I had to say the words.
“We need to let him go to the bridge.”
And with that, we made a final trip out to the vets office to be with Hercules one last time. I held him in my lap, his body just flopping over me, his eyes staring off into the distance. With Hercules’ arch nemesis (Rebecca) next to me, I consented to the procedure and gave Herc a selfless gift. I let him go to the bridge.
Unanswered questions
Hercules was gone now and the grief in the room was palpable. Myself, my husband and Rebecca were feeling the shock of having gone through such a whirlwind of events. In just over 12 hours, Hercules went from “he’s doing fine – we’re managing like we always have” to crossing the rainbow bridge.
I had so many questions. I needed to find answers to them.



